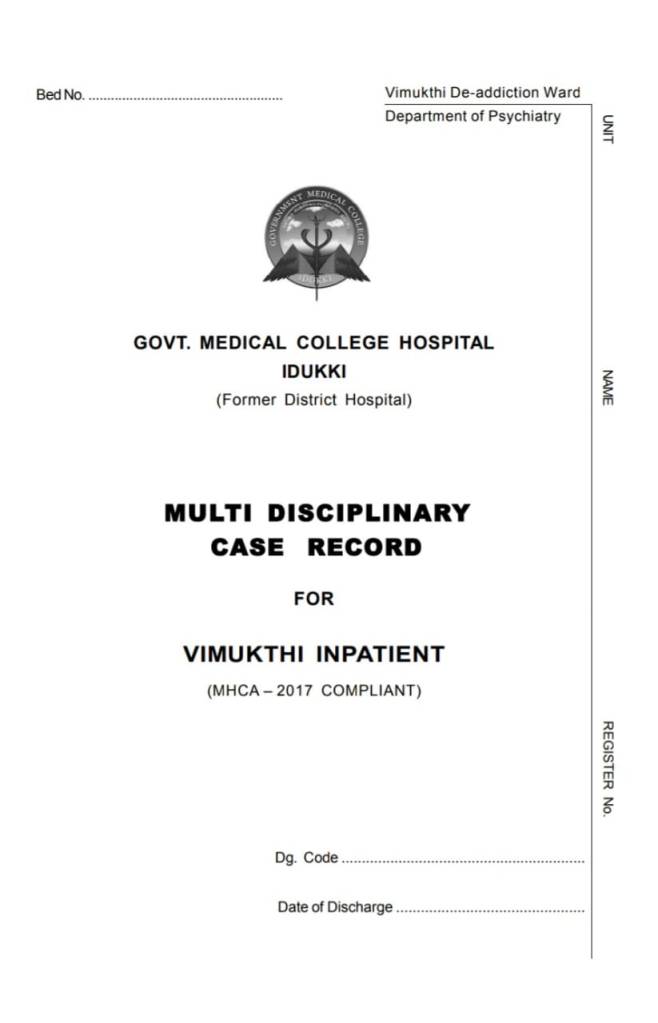
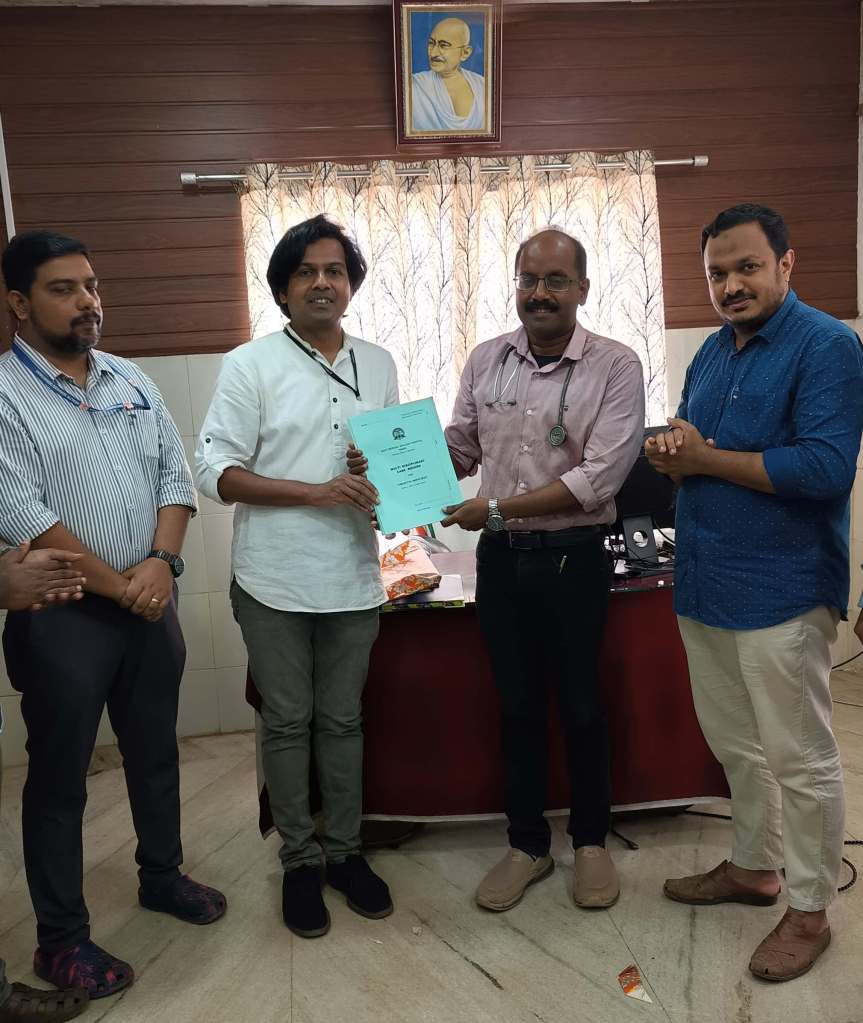
New customized IP case sheet for deaddiction (Vimukthi) launched at Idukki

Release of MHCA compliant IP case record for deaddiction ward ( Vimukthi ) by Medicine HOD Prof Renjith W in presence of RMO, Psychiatry, Vimukthi and hospital team of idukki med college .01.01.2024 11.30 AM
PDF of cover and all pages below case sheets below















Where K G George stayed?

He stayed here:
- social media – വൃദ്ധസദനം
- mathrubhoomi – വയോജനകേന്ദ്രം
- manorama – ഏജ്ഡ് കെയർ
- Indian express – care home
- thehindu – old age home
- Wikipedia – retirement home



added on 01.10.2023: related editorial on world day for elder persons in mathrubhoomi വയോജനങ്ങളല്ല അവർ വന്ദ്യജനങ്ങൾ……

Read more at: https://newspaper.mathrubhumi.com/features/editorial/editorial-1.8946057
വയോജനസൗഹൃദമല്ലാത്ത ഇടങ്ങളല്ല മറിച്ച് സമപ്രായക്കാരോടൊത്ത് സന്തോഷമായി ജീവിക്കാനുള്ള അന്തരീക്ഷമുള്ള വിശ്രമകേന്ദ്രങ്ങളും വില്ലകളുമാണ് വേണ്ടത്…….
Mathrubhoomi editorial 29 sept 2023
at 24:55 ഫാദർ ഏജ്ഡ് കെയർ സെന്റററിൽ ആണ് അതിൻറെ മലയാളം വൃദ്ധസദനം എന്നാണ്…പക്ഷേ എല്ലാവരുടെയും മനസ്സിൽ വ്യദ്ധസദനം എന്നുള്ളതിന് ഒരു നെഗറ്റീവ് ഇംപ്രഷൻ ആണ്
at 1.42 വൃദ്ധസദനം അല്ല, it is a കെയർ സെൻറർ
counter frm santivila dinesh in his channel see at 5 min …expresses the common man view ….the basis for such views is 1. can people who have relatives go into aged care ( georgesir anadhanalla) 2. who finances such care –if it is by children it puts them at a situation where conflict of interest can be alleged
mathrubhoomi archapatippu oct ist weeek: ന്യൂ ജനം വിദേശത്തേക്ക് ഓൾഡ് ജനം വൃദ്ധസദനത്തിലേക്ക് : key points : unusual comment frm adoor, home nurse vs caregiver , vridhasadanam vs geriatric care home,
home nurse vs caregiver……………………………..alludes to home nurse in the care of centenarian former CM VS (4.02 min)
https://youtu.be/1baxm0PJ6yM?si=2WW8rbSfYqN_04Rm
also to contrast with actor t p madhavan who died in same month : media projects him as lonely in care home itself . while care homes put as better for k g george
American situation worser …european would be better ? https://www.vox.com/the-highlight/23850582/millennials-aging-parents-boomers-seniors-family-care-taker
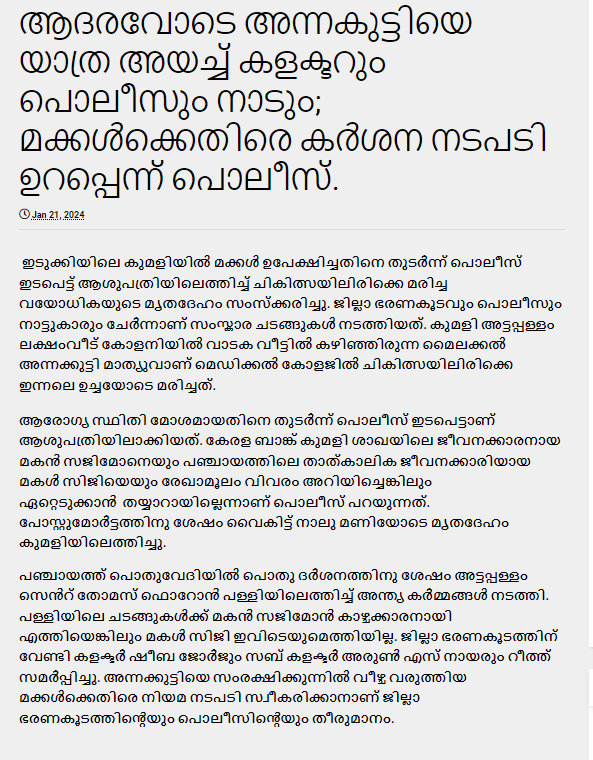
A story frm jan 2024 on twilight years: ആദരവോടെ അന്നകുട്ടിയെ യാത്ര അയച്ച് കളക്ടറും പൊലീസും നാടും; മക്കൾക്കെതിരെ കർശന നടപടി ഉറപ്പെന്ന് പൊലീസ്. https://www.honesty.news/2024/01/blog-post_31.html



added feb 2024: kudumbashree enters home care arena

ICD 11 chapter 6 on Mental behavioural or neurodevelopmental disorders PDF download
Did not find online the latest version of just the chapter 6 of ICD 11 on Mental behavioural or neurodevelopmental disorders. pdf version that i saw of chapter 6 was from the 2018 version.
Hence, here is PDF of same : covering page + chapter 6+ copyright pages as cut from the all chapter version of ICD 11 for Mortality and Morbidity Statistics (Version : 01/2023) available for download at WHO ICD11 site ( https://icd.who.int/en)
(But please note : the PDF version does not contain the many added features of online browsing like boundaries with other disorders , elaboration of diagnostic requirements, and this cut version also does not contain other chapters of direct interest to psychiatry like chapter 24 Factors influencing health status or contact with health services too.)
added frm cddr
Articles from study on psychosocial rehab homes of Kollam District published
- Residential Rehabilitation Facilities for Persons with Mental Illness: Current Status and Future Directions Based on a Survey from Kollam District of Kerala https://journals.sagepub.com/doi/10.1177/02537176211060442
- Clinical and psychosocial profile of persons with mental illness living in non-hospital residential facilities in a district in Kerala, India: A cross-sectional survey https://journals.sagepub.com/doi/full/10.1177/00207640211059678
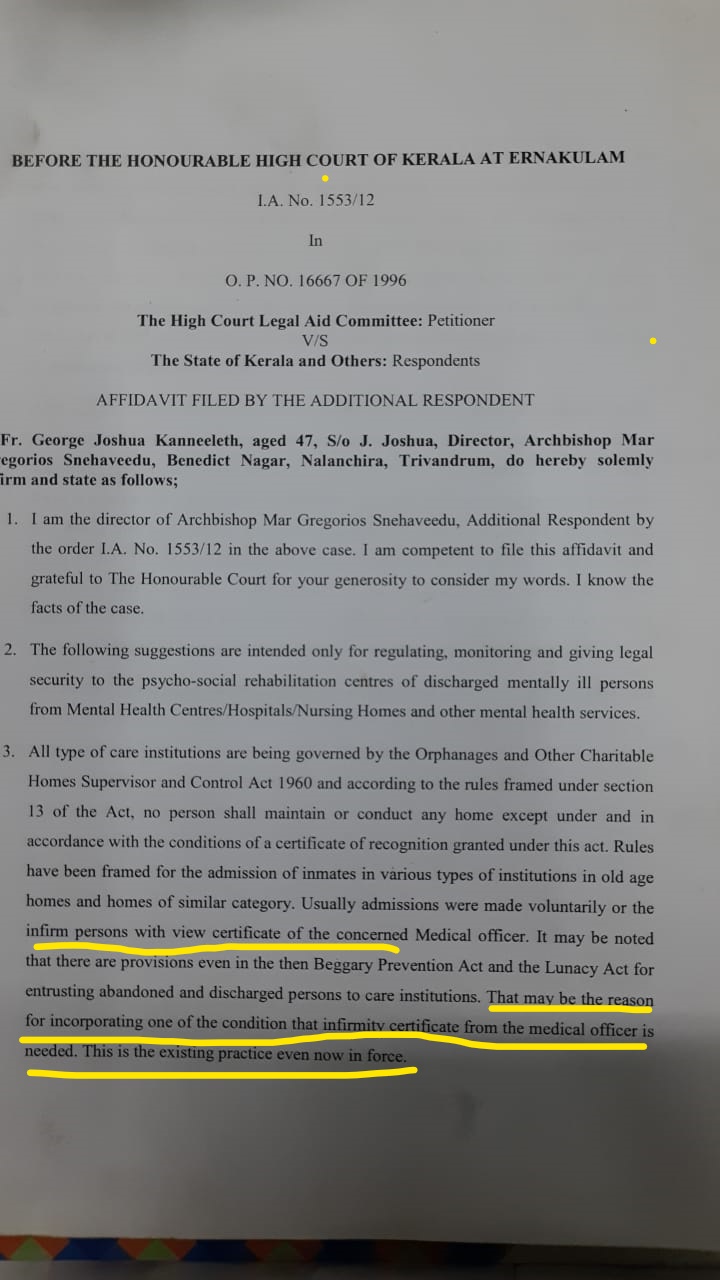
artifacts connected with this:

the End
post script:


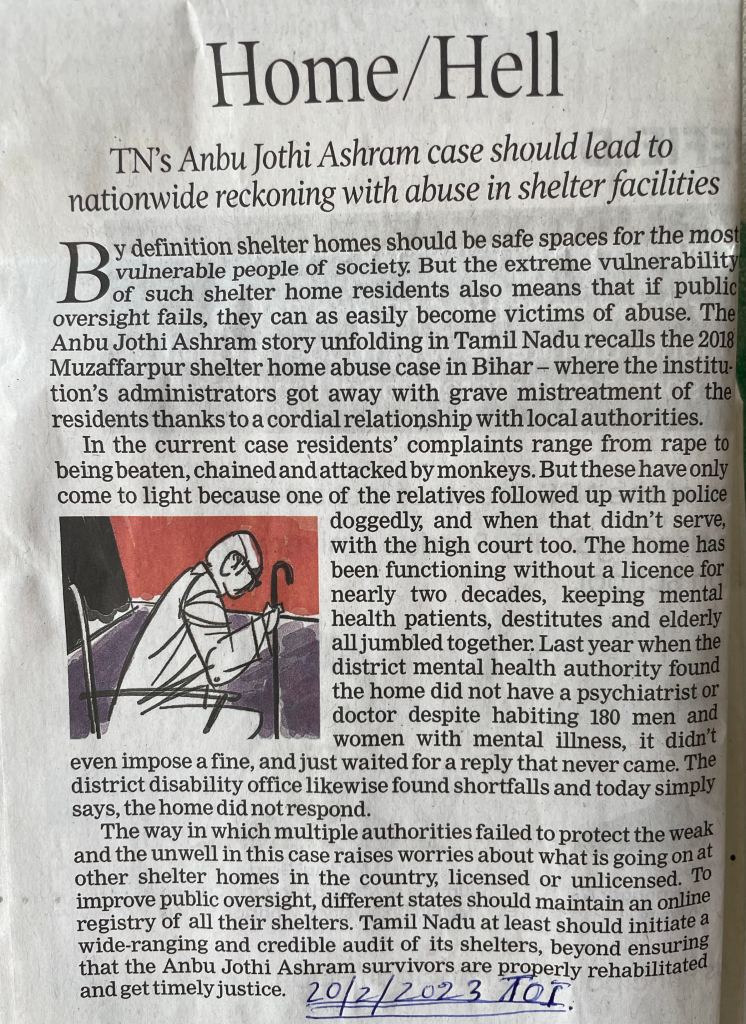
shelter situation bad in TN!
മാനസികരോഗം, മാനസികഅസുഖം, മനസികഅവസ്ഥ : the range for usage

“‘When I use a word… it means just what I choose it to mean’ Humpty Dumpty said” (Lewis Carroll, Through the Looking Glass and What Alice Found There, 1872).
First, to the controversy in April, 2019:
പ്രളയം മനുഷ്യസൃഷ്ടിയെന്ന് വാദിക്കുന്നവര് മാനസികരോഗികളാണെന്ന് താന് പറഞ്ഞുവെന്ന മലയാള മനോരമ വാര്ത്തക്കെതിരെ മുഖ്യമന്ത്രി പിണറായി വിജയന്.
Read more: https://www.deshabhimani.com/news/kerala/pinarayi-vijayan-reacts-on-malayala-manorama-fake-news/792840
Manorama reportage is challenged as follows : https://m.facebook.com/CPIMKerala/videos/1269423449871276/?_rdr
പ്രളയം മനുഷ്യസൃഷ്ടിയെന്ന് വാദിക്കുന്നവര് മാനസികരോഗികളാണെന്ന് താന് പറഞ്ഞുവെന്ന മലയാള മനോരമ വാര്ത്തക്കെതിരെ മുഖ്യമന്ത്രി പിണറായി വിജയന്.
പ്രളയകാലത്ത് കേരളം കാണിച്ച ഐക്യം പ്രത്യേക മാനസികാവസ്ഥ ഉള്ളവര്ക്ക് രുചിച്ചില്ല എന്നാണ് പറഞ്ഞത്. മാനസിക രോഗികള് എന്ന വാക്ക് മനോരമയ്ക്ക് എവിടുന്ന് കിട്ടിയെന്നും മുഖ്യമന്ത്രി ചോദിച്ചു.‘മാനസികരോഗത്തിന്റെ ലക്ഷണം നമുക്ക് അറിയാം. താന് മാനസികരോഗമെന്ന വാക്കേ ഉപയോഗിച്ചിട്ടില്ല. ഞങ്ങളെ യുഡിഎഫ് എതിര്ക്കുന്നുണ്ട്. അതിനവര് കള്ളങ്ങളൊന്നും പടച്ചുണ്ടാക്കുന്നുവെന്ന് തോന്നുന്നില്ല.
Manorama now release the original footage which contains neither usage but മാനസികഅസുഖം.
https://players.brightcove.net/5265296597001/HkxiqIeKsZ_default/index.html?videoId=6023899775001
___________________________
Now, fast forward to May, 2022 and the cycle repeats in another incident!
ശ്രീനിവാസന്റെ കിടക്കയിലെ ചിത്രം പ്രചരിപ്പിക്കുന്ന മനോരോഗികളോട്
another word : മനോ വൈകൃതം
____________________________

Added july 2022: Use of the word ‘Pandaram’ as insult is derogatory to community: Veerashaiva Mahasabha……Read more at: https://english.mathrubhumi.com/news/kerala/use-of-the-word-pandaram-as-insult-is-derogatory-to-community-veerashaiva-mahasabha-1.7741785
________________________


____________________
Added on 21.09.2022


older one :

http://dhunt.in/k8QyU?s=a&uu=0x1e4a96c81591c3dc&ss=pdSource : “Sathyam Online” via Dailyhunt
‘കണ്ണൂരിലാണേലും പുനെയിലായാലും എല്ലാ ഗവണ്മെന്റ് സെക്രട്ടറിമാര്ക്കും ഇ-ഓഫീസിലൂടെ എവിടെയിരുന്നും ഫയല് നോക്കാനും ഉത്തരവിറക്കാനും സാധിക്കും എന്ന് ആദ്യം മനസിലാക്കുക. മനോരോഗികള് അല്ലാത്തവര് വായിച്ചു മനസിലാക്കുക’-വ്യാജവാര്ത്തകള്ക്കെതിരെ ബിജു പ്രഭാകര് ഐഎഎസ്
added oct,2022 new in connection with human sacrifice
രോഗാതുരമായ മനസാക്ഷിയുള്ളവർക്കേ ഇത്തരം കൃത്യങ്ങളിൽ ഏർപ്പെടാൻ കഴിയുകയുള്ളൂ…. (emphasis added)
Read more at: https://www.manoramanews.com/news/breaking-news/2022/10/11/kerala-cm-about-elanthoor-human-sacrifice.html
more on governor vs gov : added on 27.10.2022



on name calling ..but if past is revisited!
psycho 27.11.2022

stress, depression : two discussions combined :added dec 2022


virat kohi podcast not just cricket episose talks abt depression
sibi malayil on depression
how abt others deepika padukone, criketer marshall… others
found this intersting how deshabhimani wanted to counter media response (hysterical response ) to budget2023: called it urnjuthullal



20.02.2023 “mano vikalpam” “fear psychosis”
മാനസിക രോഗി അല്ലെങ്കിൽ മനോവിഭ്രാന്തിയുള്ള ആൾ അല്ലെങ്കിൽ മയക് മരുന്നു ഉപയോഗിക്കുന്ന ആൾ



https://youtube.com/shorts/Pwe1ItNrlUM?si=BlxAUAzyjwqFDwmH
വിമർശനമുന്നയിക്കുന്നവരുടെ മനോനിലയെ കുറിച്ച് സംശയമുള്ളത് അത് വേറെ അസുഖമാണ് അതിനാണ് ചികിത്സ വേണ്ടത്
vineeth srini on addiction
അത്തരക്കാർ അറപ്പും വെറുപ്പുമുളവാക്കുന്ന മനോരോഗികൾ: പ്രതികരിച്ച് സിന്ധു കൃഷ്ണയും കൃഷ്ണകുമാറും https://www.manoramaonline.com/movies/movie-news/2023/10/17/krishna-kumar-and-sindhu-krishna-reacts-to-vluger-comments.html




28 jan 2024 manorama: പലതരത്തിലുള്ള ആരോഗ്യവും പ്രശ്നങ്ങളുമുണ്ടല്ലോ..അത് പരിശോധിക്കുന്നത് നല്ലതാണ്
feb 2024 : മദ്യപന്മാർ വരുന്നതിന് ഒന്നും ചെയ്യാൻ കഴിയില്ല
april 2024: പൂരത്തിന് രണ്ടെണ്ണം അടിച്ചിട്ട് വന്നാൽ പെടും, ആൽക്കോമീറ്ററിൽ ഊതിക്കാൻ കർശന നിർദേശം; പാപ്പാന്മാർക്കും പരിശോധന. https://www.honesty.news/2024/04/blog-post_87.html


മരണം സ്വയം തിരഞ്ഞെടുത്തത്; വിചിത്രമായ മാനസികാവസ്ഥ manorama 13.04.2024 report on manipur incident (above)
Biopsychosocial ബയോ സൈക്കോ സോഷ്യൽ
| Biological ബയോ- | Psychological സൈക്കോ | Social സോഷ്യൽ | |
| Predisposing വശപ്പെടുത്തുന്ന ഘടകങ്ങൾ Why is this person vulnerable to this problem ? എന്ത് കൊണ്ട് ഈ വ്യക്തി ഈ പ്രശ്നത്തിന് വശപ്പെടുന്നു? | |||
| Precipitating ഇപ്പോൾ ത്വരിതപ്പെടുത്തുന്ന ഘടകങ്ങൾ Why now ? ( Why is this person having symptoms now ? Why is this person presenting for treatment now ?) എന്ത് കൊണ്ട് ഇപ്പോൾ? എന്ത് കൊണ്ട് ഈ വ്യക്തിക്ക് ഇപ്പോൾ ലക്ഷണങ്ങൾ കാണുന്നു? എന്ത് കൊണ്ട് ഈ വ്യക്തി ഇപ്പോൾ ചികിത്സയ്ക്ക് സന്നിഹിതമാകുന്നു? | |||
| Perpetuating നിലനിറുത്തുന്ന ഘടകങ്ങൾ Why is this person still ill? ഇപ്പോഴും ഈ വ്യക്തി അസുഖാവസ്ഥയിലിരിക്കുന്നതെന്ത്? | |||
| Protective രക്ഷകമായ / പ്രതിരോധിക്കുന്ന ഘടകങ്ങൾ Why is this person not more ill? ഇതിലും കൂടതൽ രോഗാവസ്ഥയിലേക്ക് ഈ വ്യക്തി പോകാത്തതെന്തുകൊണ്ട്? |
പഠനവൈകല്യ സർട്ടിഫിക്കറ്റും GPay വിവാദവും മലയാളമനോരമ പരമ്പരയും
2009 മുതൽ പഠന വൈകല്യമുള്ള കുട്ടികൾക്ക് പത്താം ക്ലാസ്സ് പരീഷയ്ക്ക് ഇളവുകൾ/ സഹായം നൽകി വരുന്നു. ഇതിന്റെ ഭാഗമായി എല്ലാ വർഷവും പരീക്ഷാ സമയത്ത് എന്തെങ്കിലും വിവാദം പതിവായിട്ടുണ്ട്. അർഹതപ്പെട്ടവർക്ക് സമയബന്ധിതമായി സർട്ടിഫിക്കറ്റ് ലഭിക്കാത്തതാണ് മിക്കപ്പൊഴും കാരണം.
കുറച്ച് വർഷങ്ങൾക്ക് മുമ്പ് സർട്ടിഫിക്കറ്റ് വാങ്ങാൻ വന്ന കുട്ടികളെയും അവരുടെ രക്ഷകർതാക്കളെയും നിയന്ത്രിക്കാൻ എർണ്ണാകുളം ജനറൽ ആശുപതിയിൽ പോലിസ്സ് ലാത്തി വിശേണ്ട സാഹചര്യ തന്നെയുണ്ടായി.
ഈ വർഷമാകട്ടെ GPay യിലൂടെ ഫീസ്സ് വാങ്ങിയതാണ് വിവാദത്തിനു തിരിവെച്ചത്!


ഈ വിവാദത്തിന്റെ വശദാംശവും പഠന വൈകല്യ സർട്ടിഫിക്കറ്റുമായുമുള്ള പൊതു വിഷയങ്ങളും മൂന്ന് ദിവസത്തെ പരമ്പരയായി ശ്രീ സി കെ ശിവാനന്ദൻ മലയാള മനോരമ ദാനപത്രത്തിൽ തയ്യാറാക്കിയ പരമ്പര നല്ല വായന പ്രദാനം ചെയ്തു .
ഈ പരമ്പരയിലേക്കുള്ള ലങ്കുകളും പരമ്പരയുടെ PDF വേർഷനും താഴെ ആർക്കയിവ് ചെയ്യുന്നു.
https://www.manoramaonline.com/news/editorial/2022/01/18/problems-of-disabled-persons-series-2.html
https://www.manoramaonline.com/news/editorial/2022/01/19/story-on-special-education.html
06.03.2022 accommodations permissible in 2022.
added on 31.10.2022 concession for university exam (MG university)





pool of psychologists being created as per of initiative by disability commissioner
accomodation for teacher test SET
new media bubble on dec 2023





from karissery:

Mental Health Screening Of Arrestees/ Accused For Remand
The Judgement of the Madras high court towards mental health screening of arrestees/ accused for remand will make very informative reading as the court in this exercise resorted to a “catena of judgments, statutory provisions in the Mental Health Care Act, 2017, research undertaken until now and social commentary to make the stakeholders aware of their obligations to undertrials/ prisoners who are mentally ill.”
Hence it is added here
Related: An order from Kerala high court on prison mental health https://www.livelaw.in/pdf_upload/suo-motu-v-state-of-keralawatermark-399174.pdf
Kerala high court order on conversion therapy https://www.livelaw.in/pdf_upload/queerala-anr-v-state-of-kerala-ors-405920.pdf
06.03.2022 now SC orders screening of death row convicts too….https://www.hindustantimes.com/india-news/sc-enforces-a-landmark-ruling-on-death-penalty-101646159222001.html

sucide by remand prisoner https://www.thenewsminute.com/article/kerala-man-accused-killing-live-partner-found-dead-jail-171066
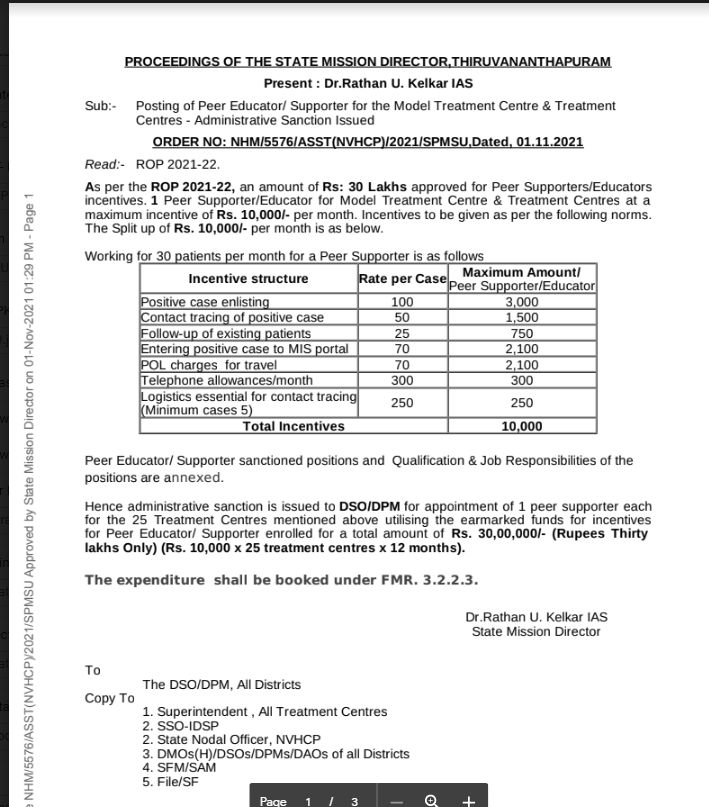
Peer Support in Mental Health
Recently came across material from the national viral hepatitis program on how it is utilizing peer support in their program.
On seeing that on Nov 2021 I commented in a professional WhatsApp group “model of peer supporter from viral hepatitis control program ……national mental health program can learn from it”
Today came across this piece from 2018 which is titled Peer support for mental illness in India: an underutilised resource. It says neither national mental health policy nor the MHCA mention peer support in mental health in India!